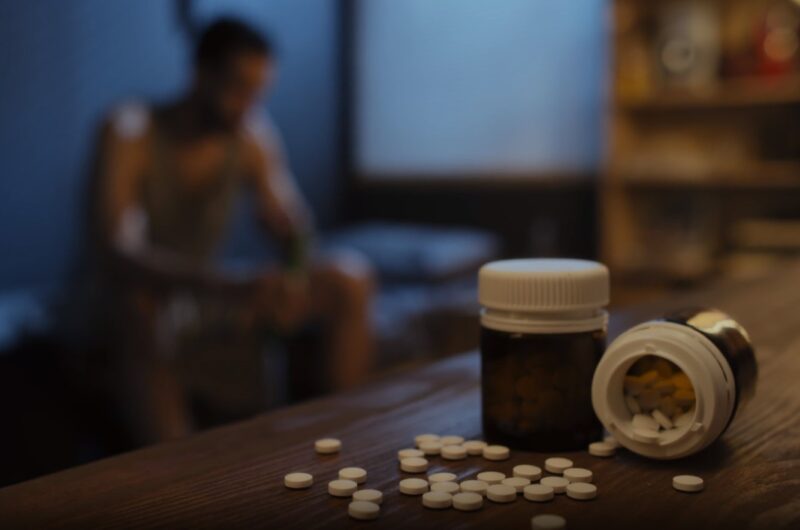
Depression and anxiety are prevalent mental health disorders that affect millions worldwide. These conditions not only impact an individual’s emotional well-being but can also have significant physical repercussions.
One such physical manifestation is erectile dysfunction (ED), a condition where a man finds it challenging to achieve or maintain an erection. The relationship between mental health and sexual function is intricate, with both psychological and physiological factors at play.
This article will explore the potential link between antidepressants, anti-anxiety drugs, and erectile dysfunction.
The Connection Between Depression and Erectile Dysfunction

Depression is a multifaceted mental health disorder that can have profound effects on an individual’s overall well-being. One of the lesser-discussed but significant impacts of depression is its potential to cause or exacerbate erectile dysfunction (ED) in men. The connection between these two conditions is both psychological and physiological.
From a psychological perspective, depression can lead to feelings of worthlessness, guilt, and a lack of interest in activities that were once pleasurable, including sexual activities. This diminished interest in sex, known as decreased libido, can be a direct result of the emotional turmoil and negative self-perception associated with depression.
Physiologically, depression can affect the body’s hormonal balance, particularly the levels of testosterone, which plays a crucial role in male sexual function. Reduced testosterone levels can lead to difficulties in achieving and maintaining an erection. Furthermore, the stress and anxiety that often accompany depression can interfere with the body’s ability to respond to sexual stimuli, further complicating the issue.
It’s essential to note that while depression can contribute to ED, it’s not the sole cause. Other factors, such as medications, other health conditions, and lifestyle choices, can also play a role in the development of erectile dysfunction.
Antidepressants and Their Impact on Sexual Function
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed medications for the treatment of depression. However, they are not without side effects. One of the most prevalent and distressing side effects associated with these medications is sexual dysfunction.
Mechanism of Action and Impact on Sexual Health
Antidepressants modulate central neurotransmitter levels, primarily serotonin, norepinephrine, and dopamine. The main classes of antidepressants include tricyclic antidepressants (TCAs), SSRIs, SNRIs, monoamine oxidase inhibitors (MAOIs), and atypical antidepressants.
Sexual dysfunction has been reported with virtually all antidepressants. The reported incidence varies considerably between studies. For instance, Rothschild concluded that 40% of individuals taking antidepressants will develop some form of sexual dysfunction. The incidence varies from 30% with imipramine to 25%–73% with SSRIs.
The mechanisms of action of antidepressants involve either inhibiting the breakdown of norepinephrine or blocking the reuptake of serotonin and norepinephrine at the presynaptic terminal, resulting in increased neurotransmitter availability at the synapse. Elevated serotonin levels are generally believed to diminish sexual function. Serotoninergic nerve terminals target dopamine and norepinephrine pathways in the brain and inhibit their activity, both of which play a role in the desire and arousal phases of the sexual response cycle.
Differential Effects of Antidepressants
Different classes of antidepressants impact all phases of the sexual response cycle to varying degrees. For instance:
- SSRIs: These inhibit the reuptake of serotonin. They are associated with a prevalence of sexual dysfunction ranging from 25% to 73%. Common side effects include decreased libido, delayed or inability to reach orgasm, and in men, delayed ejaculation and erectile dysfunction.
- SNRIs: These inhibit the reuptake of both serotonin and norepinephrine. They have a prevalence of sexual dysfunction ranging from 58% to 70%3 Side effects in men include erectile dysfunction and abnormal ejaculation, while women may experience delayed or absent orgasm.
- TCAs: These inhibit the reuptake of serotonin and norepinephrine. They have a prevalence of sexual dysfunction of approximately 30%. Side effects include decreased libido and delayed orgasm.
- MAOIs: These block the enzyme monoamine oxidase, which normally inactivates the monoamines: serotonin, dopamine, and norepinephrine. They have a prevalence of sexual dysfunction of approximately 40%. Side effects include decreased libido and delayed orgasm3.
Anti-Anxiety Drugs and Their Effect on Sexual Health
Anti-anxiety medications, commonly known as anxiolytics, are prescribed to treat a variety of anxiety disorders. These disorders can range from generalized anxiety disorder (GAD) to panic disorder and obsessive-compulsive disorder (OCD). While these medications can be effective in alleviating anxiety symptoms, they may also have implications for sexual health.
Types of Anti-Anxiety Medications and Their Mechanisms
- Benzodiazepines: These are among the most commonly prescribed anxiolytics. Drugs in this class include diazepam (Valium), alprazolam (Xanax), and lorazepam (Ativan). They work by enhancing the effect of the neurotransmitter gamma-aminobutyric acid (GABA) in the brain, leading to sedative, muscle-relaxant, and anti-anxiety effects.
- Buspirone (Buspar): Unlike benzodiazepines, Buspirone is not sedating and does not have a potential for addiction. It affects the serotonin and dopamine neurotransmitters and is specifically designed for treating GAD.
- Beta-blockers: While primarily used for heart conditions, they can also be prescribed off-label for anxiety. They block the effects of adrenaline and can help with symptoms of anxiety like trembling and rapid heartbeat.
Impact on Sexual Health
- Benzodiazepines: Chronic use of benzodiazepines can lead to decreased libido. Some users have reported erectile dysfunction, while others have experienced delayed ejaculation or anorgasmia. The sedative effects of these drugs can also lead to decreased arousal and desire.
- Buspirone (Buspar): Interestingly, Buspirone has been associated with fewer sexual side effects compared to SSRIs. Some studies even suggest it might improve sexual function in individuals who experience SSRI-induced sexual dysfunction.
- Beta-blockers: These can cause general fatigue, which might indirectly affect sexual desire. Some users have reported decreased libido and erectile dysfunction.
Studies and Research Findings

The relationship between antidepressants, anti-anxiety drugs, and erectile dysfunction has been the subject of extensive research over the years. Various studies have aimed to understand the extent and nature of this connection, providing valuable insights into the topic.
- Antidepressants and Sexual Dysfunction: A study by Rothschild (2000) published in the Journal of Clinical Psychiatry found that nearly 40% of individuals taking antidepressants reported some form of sexual dysfunction. Another study by Montejo et al (1996) in the Journal of Affective Disorders highlighted that SSRIs, in particular, were associated with a prevalence of sexual dysfunction ranging between 25% to 73%.
- Benzodiazepines and Sexual Health: Research by Longo & Johnson (2000) in the American Family Physician journal indicated that chronic use of benzodiazepines could lead to decreased libido and other sexual dysfunctions.
- Alternative Treatments and Sexual Function: Fava et al (1998) explored the effects of alternative treatments for depression and anxiety on sexual function. The research found that cognitive-behavioral therapy (CBT) not only effectively treated depression and anxiety but also had a positive impact on sexual function, suggesting it as a potential alternative or complementary treatment for those experiencing medication-induced sexual dysfunction.
Managing Erectile Dysfunction While on Medication

For many individuals, the challenge is not just managing the symptoms of anxiety or depression but also addressing the sexual side effects that come with medication. Fortunately, there are several strategies and approaches to manage erectile dysfunction (ED) while on medication.
- Understanding the Medication: It’s essential to be aware of the potential side effects of any medication you’re taking. Oral medicines for ED, such as sildenafil (Viagra), tadalafil (Cialis), and vardenafil, are often the first line of treatment for those experiencing difficulty in getting or maintaining an erection. These medicines enhance the effects of nitric oxide, a chemical that relaxes muscles in the penis, boosting blood flow and aiding in achieving an erection during sexual activity.
- Communication with Healthcare Providers: Always discuss any side effects you’re experiencing with your healthcare provider. They can provide guidance on potential medication adjustments or alternative treatments. For instance, if you’re on a specific antidepressant causing ED, your doctor might consider switching you to another medication with fewer sexual side effects.
- Lifestyle Changes: Some lifestyle changes can help manage ED. This includes maintaining a healthy weight, avoiding excessive alcohol consumption, quitting smoking, and engaging in regular exercise. These not only improve overall health but can also enhance sexual function.
- Therapeutic Interventions: Cognitive-behavioral therapy (CBT) has shown promise in treating depression and anxiety and has a positive impact on sexual function. This suggests that therapy can be a complementary treatment for those experiencing medication-induced sexual dysfunction.
Alternatives and Solutions

While prescription medications like SSRIs and benzodiazepines are common treatments for depression and anxiety, they are not the only options available. For those who experience side effects or are seeking alternative treatments, there are several natural and holistic approaches to consider:
Lifestyle Changes
- Sleep: Adequate sleep is crucial for emotional well-being. Maintaining good sleep hygiene, such as consistent bedtimes, a relaxing bedtime routine, and avoiding screens before sleep, can help improve mood.
- Diet: Consuming a balanced diet rich in nutrients can influence mood. Foods like fish, which are high in omega-3 fats, have been linked to reduced symptoms of depression. Additionally, nuts and probiotics can also play a role in mood regulation.
- Exercise: Regular physical activity can improve mood and quality of life. Even low-intensity activities, such as walking, can be beneficial.
Natural Remedies
- St. John’s Wort: This herb has shown effectiveness in relieving symptoms of mild-to-moderate depression.
- SAM-e and 5-HTP: These dietary supplements may help reduce depression symptoms, but it’s essential to use them cautiously due to potential side effects.
- Vitamin D: A deficiency in vitamin D might be linked to depression. If you aren’t getting enough from your diet or sun exposure, consider a supplement.
Mindfulness and Meditation
Mindfulness-based cognitive therapy (MBCT), which combines elements of cognitive behavioral therapy with mindfulness meditation, has been found effective in treating depression and preventing symptom relapses.
Social Connections
Engaging with loved ones, joining support groups, or volunteering can help combat feelings of isolation and loneliness, common in depression.
Cognitive Behavioral Therapy (CBT)
This form of psychotherapy focuses on identifying and changing negative thought patterns, making it a popular and effective treatment for depression.
Seeking Professional Help

Addressing erectile dysfunction (ED) and its potential link to medications for depression and anxiety is not a journey one should embark on alone. Professional guidance is paramount in navigating these intertwined challenges.
- Consultation: If you’re experiencing ED, especially if it’s sudden or severe, it’s crucial to consult a healthcare professional. They can help identify the underlying cause, whether it’s related to medication, psychological factors, or other health conditions.
- Open Dialogue: When discussing ED with a healthcare provider, it’s essential to provide a comprehensive medical history, including any medications currently being taken. This will help the provider determine if there’s a link between the medication and ED.
- Adjustment of Medication: If it’s determined that medication is the likely cause of ED, the healthcare provider might consider adjusting the dosage or switching to another medication with fewer sexual side effects.
- Therapeutic Interventions: For some, therapy can be beneficial. Cognitive-behavioral therapy (CBT) can address both depression and anxiety, potentially alleviating some of the psychological factors contributing to ED.
- Referral to Specialists: In some cases, a primary care provider might refer an individual to a urologist or a mental health professional for specialized care.
FAQ
What is Post-SSRI Erectile Dysfunction?
Post-SSRI Erectile Dysfunction (PSSD) refers to persistent sexual side effects that continue after discontinuation of selective serotonin reuptake inhibitor (SSRI) medications. These side effects can include erectile dysfunction, reduced libido, and other sexual dysfunctions. The exact cause of PSSD is not fully understood, but it’s believed to be related to changes in brain chemistry and function induced by SSRIs.
Are there specific antidepressants known to cause fewer sexual side effects?
While many antidepressants can cause sexual side effects, some are associated with a lower risk. For instance, Bupropion (Wellbutrin) is often considered to have a lower risk of sexual side effects compared to other antidepressants. Additionally, Mirtazapine (Remeron) and the aforementioned Buspirone (Buspar) are also reported to have fewer sexual side effects. However, individual responses can vary, and it’s essential to discuss any concerns with a healthcare provider.
Are there any non-prescription supplements or herbs that can help with erectile dysfunction?
Several non-prescription supplements and herbs are often touted as treatments for ED. Some of the commonly mentioned ones include L-arginine, Panax ginseng, Rhodiola rosea, and Yohimbe. While some studies suggest these might have potential benefits, the evidence is not robust, and their safety and efficacy are not well-established. It’s essential to consult with a healthcare provider before trying any supplements, as they can interact with other medications and have potential side effects.
Conclusion
The intricate relationship between depression, anxiety, their treatments, and erectile dysfunction underscores the importance of holistic care. While medications can be life-changing for many, they might come with side effects that affect one’s quality of life.
It’s essential to be proactive, seek professional guidance, and explore both medical and non-medical solutions. Remember, you’re not alone in this journey, and help is available. Don’t suffer in silence; reach out and take the first step towards a healthier, happier life.
